Pain Management Versus Spinecare?
 As I started to put together our next SpineCare Newsletter, I noticed that one of the main topics in the news these days is the prescribing of narcotics by physicians for pain management and the subsequent drug addiction and overdoses this creates. Take for example the singer Prince.
As I started to put together our next SpineCare Newsletter, I noticed that one of the main topics in the news these days is the prescribing of narcotics by physicians for pain management and the subsequent drug addiction and overdoses this creates. Take for example the singer Prince.
As of 2011, 75 percent of the world’s narcotic prescription drugs were prescribed and swallowed up in a country that makes up less than 5 percent of the world’s population, leading to the most common cause of preventable death in America today. Millions of Americans are addicted to narcotics and in 2013 alone prescription narcotics were involved in 37 percent of all drug overdoses. Starting in the 1990’s, there was a dramatic increase in the use of narcotic painkillers by physicians to treat non-cancerous medical conditions like low-back pain, sciatica and various musculoskeletal problems. There is almost no evidence to show that narcotics are safe or effective for the long-term management of non-cancerous pain, even though they are very effective for the relief of short-term pain.
Patients who take narcotics for periods as short as 3 weeks may actually have hypersensitivity to pain, a condition known as “narcotic hyperalgesia.” These patient’s actually have more pain than if they had not taken the narcotic to begin with. Patients also develop a tolerance to these medications. Over time narcotics appear to become less effective, and therefore you have to take higher and higher doses to obtain pain relief. We know this leads to overdoses and death. Now all of a sudden, the medical community, which created the current narcotic epidemic with their backing of the use of long term narcotics, is trying to figure out how to control non-cancerous pain like low-back pain and sciatic pain without the use of narcotics. One of the leading experts in pain management now says “that physicians need to create unique treatment options other than narcotics to effectively treating chronic pain”. These so called experts are still missing the boat. What you have to do is eliminate the pain before it becomes chronic! If you eliminate the pain there will be no need for narcotics.
We at SpineCare have watched this whole process go on over the last twenty years. Our physicians and nurse practitioners never bought into the pain management idea as we felt a better service to the patient would be to diagnose the exact problem causing the pain, and then attempt to treat this underlying problem by eliminating the painful inflammation. If we fail, we get you into the right hands to fix the problem. Diagnose the problem and treat the problem directly instead of just masking it with narcotics.
Have you ever wondered why we don’t use the words Pain Management in our company name? Why we never prescribe long-term narcotics? The reason is because we have the ability to diagnose and locate the inflamed structures in the spine and eliminate the inflammation. No inflammation, no pain. No pain, no narcotics.
This is where the problem with the pain management community lies. If you cannot or do not know how to locate the specific spinal structure that is creating the pain and treat the problem, the pain will not go away. If the pain does not go away, then these physicians resort to trying to cover it up with narcotics. Once that happens, it is very hard to get the patient off the narcotics. Why? Because narcotics actually alter the structure of your spinal cord and produce something mentioned earlier in this article called “hypersensitivity” to pain. Your body’s perception of pain is increased and that means that for a given injury, it will hurt more than if you were not taking the chronic narcotics. Additionally, because of what narcotics do the brain and spinal cord, treatments that would normally work and improve your pain will no longer be effective. These alterations make it very difficult to get a person dependent on narcotics to give them up.
While the government has mandated drug testing in clinics like ours, this has helped us to identify patients at risk for failed treatments. We have patients come to see us who would fail to tell us that they were on narcotics. When our procedures did not give them relief and we later found out that it was because they had been on long-term narcotics we would recommend detoxification, however this was often to late. With failure to respond to the treatment, these patients would frequently demand more pain medications that we recommend against. Needless to say, these patients typically are none too happy with us when we refuse to provide the medications and recommend detoxification. They had become dependent on narcotics before seeing us through no fault of our own. This frequently explains why good physicians can get poor scores on physician on-line rating services. The good news is that since we started drug testing everybody, we can pick out these patients that do not tell us about their narcotic usage before we treat them with our procedures and this has made our treatment much more reliable.
The bottom line is that we do not want our patients dependent upon narcotic medications before we treat them. What is chronic? Over 3-4 weeks. It has been shown that narcotics are very effective for short bouts of severe pain for around 2-4 weeks. The chance of addiction and hypersensitivity occurring is minimal during this time.
As mentioned earlier, what separates us from the pain management crowd is our ability to locate and treat the inflamed structures in the spine. Our specialized interventional procedures cannot only diagnose the offending structure causing pain, but are also used to treat these specific areas. If you do not have the training or experience needed to find and treat the area in your spine that is inflamed, there may be no relief from the injection. Injecting the spine in an area that is not causing the pain or that is not inflamed will not produce good results.
Lets show you an example of what we are talking about, but first lets look at the parts of the spine.
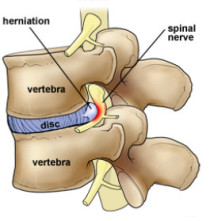
Figure 1 – You can see in the picture to the left the three main parts of the spine that can become inflamed. These are the disc, the nerve, and the facet, which is the joint in the back of the spine. To eliminate the inflammation and the pain you have to place the anti-inflammatory medication exactly on the inflamed area. If the medication does not reach the specific area of inflammation you will not obtain relief.
Figure 2 – The patient had a pain diagram. Now lets give you an example. A recent patient had a disc herniation in the neck that was pressing on a nerve causing pain going down the arm.
The patient should have had medication placed directly on the nerve where the disc herniation is pushing against it. The procedure to have this done is called a Nerve Root Block or Transforaminal Injection. As you can see in the picture below the steroid is placed directly on the disc and nerve where the inflammation has occurred.
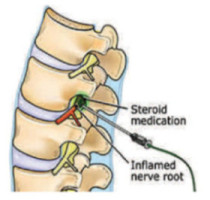
Figure 3 – This procedure is done from the side of the neck as it is very easy to get to this nerve from that direction, and it is very safe as the needle is placed outside of the spinal canal away from the spinal cord and only the liquid medicine goes to the inflamed disc and nerve.
 Figure 4 – Instead, this patient had a series of epidural steroid injections at another facility. Epidural steroid injections are done from the back of the spine. The needle is directed into the spinal canal heading directly towards the spinal cord. As you can see in the picture below, the needle ends up very close to the spinal cord and the medication travels in the the back of the spinal canal while the disc is in the front of the canal. Additionally, the liquid medication will travel the path of least resistance medication away from the swelling at the disc and nerve. The result was that this patient did not get much better even after a series of three epidurals.
Figure 4 – Instead, this patient had a series of epidural steroid injections at another facility. Epidural steroid injections are done from the back of the spine. The needle is directed into the spinal canal heading directly towards the spinal cord. As you can see in the picture below, the needle ends up very close to the spinal cord and the medication travels in the the back of the spinal canal while the disc is in the front of the canal. Additionally, the liquid medication will travel the path of least resistance medication away from the swelling at the disc and nerve. The result was that this patient did not get much better even after a series of three epidurals.
Why is this approach still used? Because there are a lot of physicians that never trained to used the cervical nerve root block and therefore they still use a procedure the older cervical epidural steroid injection. Which is only about 20% effective compared to 70% with the transforaminal nerve block technique. After one cervical nerve root block on this patient she has had complete relief of her pain.
Do not get the wrong idea about this! This patient may have not had relief from the cervical nerve root block, but why not give her the best chance and safest way to get better?? Even if she did not get long term relief, the procedure has now identified the exact source of her pain with imaging to help with surgical planning.
There are anesthesiologists, neurologists, surgeons and physical medicine doctors that are doing procedures without any special training after their residency except for weekend courses. As it is difficult to learn the technique of doing a cervical nerve root block over a weekend on a cadaver, these physicians prefer to do epidurals even though they are not the most effective way to treat an inflamed nerve. All of the physicians at SpineCare did a fellowship AFTER their primary training so that we could provide the highest level of care and have all had over twenty-five years of experience performing these technically challenging diagnostic and therapeutic procedures.
We have many patients that come into our offices and tell us that they have had multiple injections with no relief, and we have to spend hours explaining how we do things differently. One important point to make – If you are going to have a pain management procedure, the physician performing the procedure for a copy of the report along with the saved x-ray images of the procedure. You may find that most physicians, for some reason, do not save any x-ray pictures from their procedures. At SpineCare, we always save pictures on all procedures so that you can see exactly what we did, and where we placed the medications. It should tell you something if the physician that you are using does not keep the x-ray pictures from their procedures.
In summary, it is of utmost importance that you get an accurate diagnosis of the exact structure causing your pain and not just a guess based on an MRI alone. The more accurate your diagnosis, the more accurate the treatment. Your treatment needs to be directed specifically and effectively to the inflamed source of your pain and not just in the vicinity if you are going to get any relief. Avoid at all costs just masking your pain with narcotics as this is a very slippery slope that can lead to dependence, increased pain and even death.


